Well-Placed
In the face of exclusion and displacement, how do communities mobilize urban space for mental health and collective wellbeing?
We are celebrating 15 years — and counting — of stories that are deeply researched and deeply felt, that build a historical record of what the city has been.
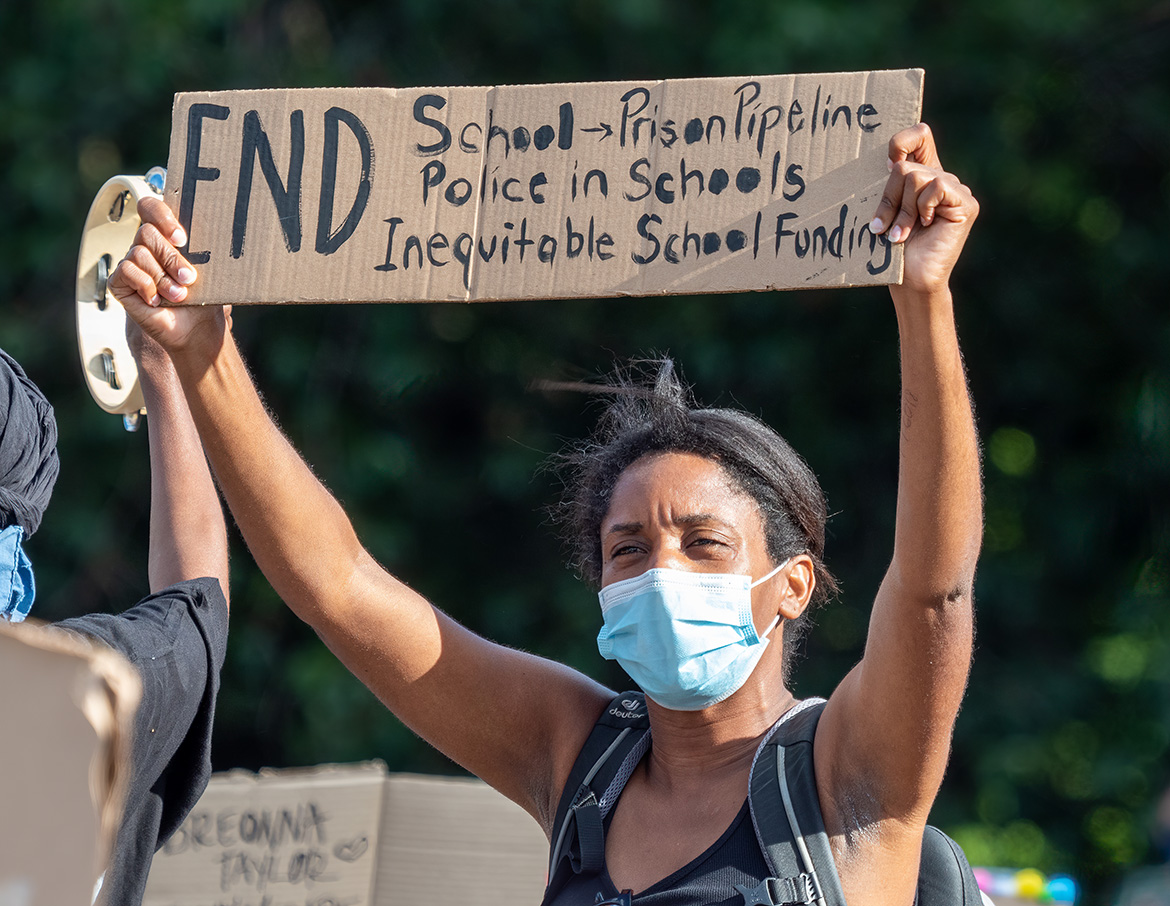
Jordan Neely’s murder on May 1, 2023, is a reminder of the urgency with which New York City’s government needs to support and protect the lives of New Yorkers with the greatest needs. An unhoused Black man with mental health challenges, Jordan Neely cried out before his death that he needed food, water, and housing. Like so many people living with mental illness, he became a victim of violence rather than receiving the care he needed. Dr. Michael McRae’s insights from this interview conducted in April 2023 are timely, as New Yorkers seek to understand the crisis in mental health care and imagine a city that does not criminalize, dehumanize, or perpetrate violence against its people, but is committed to compassionate care.
What does mental healthcare look like from a citywide perspective? For the final installment of our Well-Placed series, we explore the challenges of running large, broadly accessible programs that are malleable enough to meet the needs of diverse individuals and communities. Working amid a mental health crisis exacerbated by systemic racism, housing insecurity, the Covid-19 pandemic, and the criminal legal system, Dr. Michael McRae has designed programs and interventions to support mental health and well-being on behalf of New York City’s Department of Health and Mental Hygiene and the nonprofit START Treatment and Recovery Centers.
Mental healthcare comes in many forms — and Dr. McRae is not satisfied with only traditional options. Below, he emphasizes the need for creative approaches to mental healthcare on a citywide scale. New Yorkers who have experienced mental health-related trauma deserve love and pampering, Dr. McRae argues. Exploring new possibilities, Dr. McRae supports the expansion of “clubhouse model” social resource centers that allow the people they serve to feel a sense of ownership over a space. He urges public health professionals to make connections between mental health and the places we live, play and work, and between housing and food insecurity and mental health. He also advocates the centering of community-building activities alongside medical and social support. This interview explores what equitable care across the city could look like. – RJ
You’ve had an extensive career in mental health. Can you share a bit about yourself and why you decided to go into this work?
I’m a clinical psychologist by training. I’ve always been a person who is interested in other kinds of social interactions and helping people. I went to the Historically Black University Morehouse College in Atlanta, where I first I started getting involved in research in psychology. I went on to graduate school and became a clinical psychologist, with a focus in the areas of assessment, forensics, and developmental psychopathology. I began my career at the Federal Bureau of Prisons, performing forensic evaluations for pretrial detainees with serious mental illness and/or those suspected of being incompetent to stand trial. Since then, I’ve found myself working with people and communities that have been impacted by the criminal legal system. More recently, as acting Executive Deputy Commissioner for the Division of Mental Hygiene with the City’s Health Department, I was responsible for overseeing the department’s mental health and substance use policy, programming, research and data, and mayoral priorities like the asylum seeker and subway initiatives. Now, as the Chief Program and Strategy Officer at START Treatment and Recovery here in NYC, I am returning to my love of working to improve health outcomes of the most marginalized communities. The mental health crisis we are experiencing requires an all-hands-on-deck approach, so I am especially grateful for the opportunity to be on the ground, in this space, at such a critical time.
What role have equity and social justice played in your work?
I’ve always been driven to work with people who are marginalized, much like myself, a Black male who grew up poor. Many people in my life have experienced mental health and substance use challenges, and to me, much of it was about health inequity, the racist “War on Drugs,” and so forth. Health equity is about recognizing and rectifying some historical injustices. And then making sure that people have resources according to what they actually need and want.
Health disparities will only be eliminated when health equity is achieved. Interestingly, if you look at the redlining maps from the city from the ‘30s, you see we have glaring similarities between those maps where people could not get mortgages and present-day health inequities. We see that with substance misuse, overdose deaths, mental health conditions, criminal legal system involvement, and so many more health outcomes, disproportionately impacting people who are marginalized, most often Black and brown people. I think we have an obligation to really make sure everyone has the same level of access, and that requires giving more resources and support to people who need it in order to live happy, healthy lives. If you don’t have a stable place to live and food to eat, it’s really hard to focus on self-actualization. So my intention or my passion around health equity is to make sure that everyone has adequate access, regardless of where you come from.
How has the Covid-19 pandemic and response to it impacted the mental health of New Yorkers?
I remember the early days of the pandemic, the trauma of it all. Late nights, all you heard were sirens, and it was a kind of a ghost town, which is so different for New York City. So many experienced loss, including youth, who already experience challenges. Many youth lost both parents, or multiple family members. We were told to stay away from others. The cumulative nature of all this trauma has definitely had a definite impact on the mental health of New Yorkers.
The City’s health department put out an EpiData brief in December of 2021, and up to 25 percent of adults experienced probable anxiety over the past two weeks, and 20 percent probable depression. Almost 30 percent of all parents said that Covid-19 had negatively impacted their children’s emotional or behavioral health. And that’s all elevated from pre-pandemic levels. Calls to the mental health hub, NYC Well, shot up, so people were looking for that extra support. Since the pandemic, we’re also seeing a historic rise in overdose deaths as well. Definitely, all the trauma of the pandemic is showing itself, in so many different ways.
And we’re still living through the figuring out how much healing can be done, and what will come of it. And how much has been forgotten or how much can actually be addressed for people.
During the pandemic, there was also a lot of social unrest, and there continues to be that in our politics. That also impacted people’s mental health, in terms of the feeling of safety, belongingness, and loneliness. It’s very challenging to disentangle it, you know?
How can specific institutions tasked with supporting mental health, like hospitals, schools, community centers, and other spaces, be improved to actually help people?
We often talk about access to health care, but I think that it’s really about making sure services are available, accessible, and acceptable. One of my former health department colleagues really drilled down on this, but it is quite accurate. We have to ensure that all people have access to high-quality services. People who are interacting with these institutions, like hospitals, schools, and community centers, oftentimes have very complex trauma, lives, and challenges. Institutions have to be able to provide services and support that people need and want. There is some discussion around clinical algorithms physicians use, that have some kind of impact in terms of how different people are assessed, treated, and cared for. These are troubling algorithms that some clinicians use that end up really disproportionally impacting Black and brown people. So, I think there’s a change in mindset, there’s stigma reduction, making sure these places are just prepared to know and appreciate the people that they’re interacting with, appreciate their experience and trauma.
In March of 2023, New York City Mayor Eric Adams and New York City Department of Health and Mental Hygiene Commissioner Dr. Ashwin Vasan announced a new mental health plan for the city called “Care, Community, Action: A Mental Health Plan for New York City.” What are your thoughts on this new mental health plan?
I was very much involved with leading the mental health work from the health department side. This plan is comprehensive, and it’s the largest plan we’ve ever had for the city. It crosses multiple sectors of city government and partnerships, and it focuses on three groups of New Yorkers with the greatest need: children, youth and families, people with serious mental illness, and people who are at risk of drug overdose. It offers concrete investments in all three of those areas. We know that youth and families are hurting. People with serious mental illness need access to specialty care and housing and are hurting. We know the community of people who use drugs are hurting.
We also know that we’re seeing an unprecedented number of overdoses in the city. The data is staggering. 2,668 souls perished in 2021 as a result of an overdose. And we anticipate this will be even higher once the 2022 data is finalized. In 2019, there were 1,500. Those are heavily concentrated in the Bronx and Harlem. The data is saying that Black and Latino New Yorkers experienced the sharpest increase in deaths involving fentanyl. I think about the city’s investment in harm reduction as a strategy. We have 15 syringe service providers in the city. Part of the plan will include additional funding for these programs to become hubs and places that offer a wide range of services. A one-stop shop, if you will.
They’ve been investing in clubhouses. Clubhouses are places for people who have serious mental illness to go to engage in meaningful, everyday activities. They are for people who have been disenfranchised from many different sectors and join to encounter and build community. They take ownership in how the place functions, they cook in the kitchen, they are the community. They can connect in to different services they want and need.
There’s no perfect plan, but I think it is promising that the plan does offer some concrete investments for community-based organizations like my organization, START Treatment and Recovery.
How could New York City’s agencies and government better support the mental health and wellbeing of its residents? Are there any examples that we could learn from elsewhere that you think are really incredible and worth trying to replicate?
New York City government is very complicated. There has been a lot of focus and effort on increasing the efficiency of government, but I think in the end, it’s about making sure people’s basic needs are met and addressing their social determinants of health. These are conditions and environments where people are born, where they live, learn, work, play, pray, worship — that really affects our health, our functioning, our quality of life. Again, if you don’t have a roof over your head, or you’re food insecure, that’s going to impact your mental health and motivation and happiness in life.
I take my social determinants of health work from Healthy People 2030. The five different areas are economic stability, educational access and quality, healthcare access and quality, the neighborhood and built environment, and the social and community context. I think the city government has an obligation to make sure all people have access to all of these and to redress some of the harms that have been done over time.
One of the models that I am a particular fan of was a model that I helped grow from inception in Los Angeles: the Office of Diversion and Reentry. Basically, community members were coming home from jail or prison, and were experiencing homelessness as well as mental health and/or substance use challenges. What the Office of Diversion and Reentry was offering was temporary, interim housing, with the goal of permanent, supportive housing. They were offered intensive case management services to help connect people to services they need. So to me, it’s housing and wraparound services, including those intensive services, that is really key.
We can start similar work here at START with the support from city, state, and our philanthropic partners. It would be great to be able to offer housing and really robust clinical wraparound services, medication support, and access to wellness opportunities as well. It’s not just about clinical services, but how about massage, and acupuncture, Reiki, and other holistic forms of care that contribute to one’s healing. I think people who are experiencing homelessness, mental health challenges, substance use issues, coming home from jail a prison, they deserve to be pampered even more and shown love and support by us all, including government, you know? That’s equity, right? It’s really giving them the boost they need to feel good about themselves or to live happy, productive lives, and to ultimately thrive.
The views expressed here are those of the authors only and do not reflect the position of The Architectural League of New York.
In the face of exclusion and displacement, how do communities mobilize urban space for mental health and collective wellbeing?