We are celebrating 15 years — and counting — of stories that are deeply researched and deeply felt, that build a historical record of what the city has been.
We are celebrating 15 years — and counting — of stories that are deeply researched and deeply felt, that build a historical record of what the city has been.
As the city seeks to reopen after months of lockdown, there is a creeping sense that too many New Yorkers may be losing the will to look out for their most vulnerable neighbors — and no, don’t blame the protestors. The pandemic’s disproportionate burden on working-class people of color has led some to cruelly dismiss COVID-19 as largely “a Black and brown problem.” Meanwhile, even as thousands of coronavirus survivors struggle with slow, painful recoveries, the perception that only older adults are at risk of severe illness and death has fostered a false sense of security among the young and healthy. The abdication of social responsibility is itself an emerging disaster, and the particular risk to elderly New Yorkers is so great that it may just constitute a form of age discrimination.
Across the US, this crisis of care is potently illustrated by a grim statistic: More than one in three coronavirus deaths have been linked to nursing homes. The slow and uncoordinated response at all levels of government in protecting residents and their caretakers has only reinforced the stereotype that such facilities are “forgotten” places. It does not have to be this way. Below, Willa Granger shows how the history of the New Jewish Home, with roots in Manhattan stretching back more than 150 years, indexes an enduring tension between medical and social needs in “homes for the aged.” Unlike many senior care facilities, the Home never left New York, even as threats of contagion and theories of suburban salubrity led other institutions to relocate. The importance of integrating facilities with their wider communities and fostering opportunities for intergenerational exchange has never gone away. While physical reconnection may not be yet possible, building more durable bridges between the city and its elders will be an essential infrastructure of empathy long after the worst is over.
The New Jewish Home is on lockdown. Visitations for family and friends have been suspended indefinitely. The Home’s Manhattan branch has even had to limit deliveries of essentials, such as laundry: Every person, let alone every object, is a potential conduit for the COVID-19 virus to wreak havoc on vulnerable seniors within. The worst-case scenario has already happened. To date, there have been 46 confirmed COVID-19 related deaths at the facility.
Book-ended by the Duke Ellington Gourmet Deli on one side, and the NY Brat Factory on the other, the New Jewish Home’s Manhattan campus occupies the street-face of nearly an entire city block on the Upper West Side. Pre-pandemic, the Home was a backdrop to typical New York scenes: busy with pedestrians, with scaffolding along its façade, and staff congregating at the front entrance between shifts. The facility can house up to 514 residents, including short-term rehabilitation patients (those in need of recuperation and physical therapy after surgery) as well as long-term nursing patients, whose needs for care are so complex that they can no longer live independently at home. Beyond the ministrations of everyday life, the Home provides a busy programming schedule, including bingo, book club, adapted yoga, creative writing, and glee club rehearsal — not to mention a smorgasbord of religious services, as the Home is no longer exclusive to Jewish residents alone. The facility accepts Medicare and Medicaid reimbursements, which means that some percentage of its patients are low-income. Sheltered care often gets a bad rap for serving the affluent alone, but this is not so at the New Jewish Home of Manhattan.
The nomenclature for a facility such as this one is varied: nursing home, long-term care facility, or, more pejoratively, an “old folks’ home.” Nurses, doctors, therapists, social workers, and chaplains roam the halls; uncarpeted flooring, often graded at a smooth incline, accommodates the many wheelchair users; beds are equipped with call buttons and grab bars. Despite these features, the New Jewish Home has found tasteful strategies to minimize the “institutional” aesthetics, such as applying pendant fixtures instead of ceiling panel lights, or replacing linoleum tiles with laminate wood flooring. But even these design flourishes cannot wholly obfuscate that the building complex is medical in nature.
Today we recognize that heavy-handed healthcare can be detrimental to the psychic and emotional needs of seniors who wish to simply live their lives in whatever capacity they can. As contemporary nursing homes work to keep seniors protected, the coronavirus crisis has stymied any attempt at fostering a good, let alone “normal,” quality of life for older adults. And though it is reasonable to decry the over-medicalization of senior homes, in which the New Jewish Home has certainly played a part, the COVID-19 lockdown has also thrown into relief just how difficult it is to juggle the question of integrating and segregating vulnerable seniors within a wider community.
The COVID-19 crisis is, in many ways, a spatial issue. Human proximity is one factor (among others) that can speed the virus’ transmission, and commentators have latched onto the city’s density as key to its rapacious infection velocity. Senior care homes are no exception to this vulnerability. At once necessary for chronically ill and non-ambulatory patients in need of skilled care, nursing and old age facilities run the risk of making outbreaks worse by congregating large populations of vulnerable older adults in a confined setting. Seniors are at a higher risk of succumbing to the virus, whether living independently or in congregate settings.
The numbers attest to this. Italy, one of the hardest-hit countries in Europe, also has the second oldest population of any nation — a fact that likely contributes to its elevated coronavirus death rate. This reality was laid bare when the first COVID-19 outbreak arrived on American soil: in a Washington State nursing home, no less, where the virus quickly spread amongst staff and elderly residents, ultimately killing 37 of its occupants. Already “homebound,” residents of nursing homes or senior care facilities are currently living, in the words of one headline, in “islands of isolation” amidst the outbreak. Medically, this is necessary, but as the child of one nursing home resident put it, “I’m concerned that the loneliness and helplessness will kill her quicker than the virus.” These past weeks have revealed how that loneliness and helplessness goes both ways, as family members have been unable to say goodbye to their dying loved ones, or to mourn through proper burial. It is now estimated that one-third of all coronavirus deaths in this country have occurred amongst nursing home residents or staff.
The tragedy at the Life Care Center of Kirkland, Washington — and now other senior facilities across the country, including the New Jewish Home — reveals the imbrication of aging and architecture. For those approaching advanced old age, life is tethered to a distinct spatial and material reality: The number and distance of daily steps become measured, the ability to operate a vehicle can be reneged, and even the ability to reach or bend towards cabinetry and furniture is diminished. Widespread social distancing, ironically enough, has compelled youngsters to occupy a confined existence common to many seniors who live in isolation without access to transportation, or bound by disability and chronic disease to a sheltered setting. Even though the able-bodied still have recourse to daily walks, jogs, and occasional grocery visits, this time has been logistically and emotionally trying for many. But old age institutions, struggling to provide shelter for seniors, have likewise had to seek strategies to combat contagion. And they have always, even before modern medicine (let alone germ theory), operated largely according to a unique spatial logic, privileging low-density locales divorced from the hazards of the crowded, pre-car city.
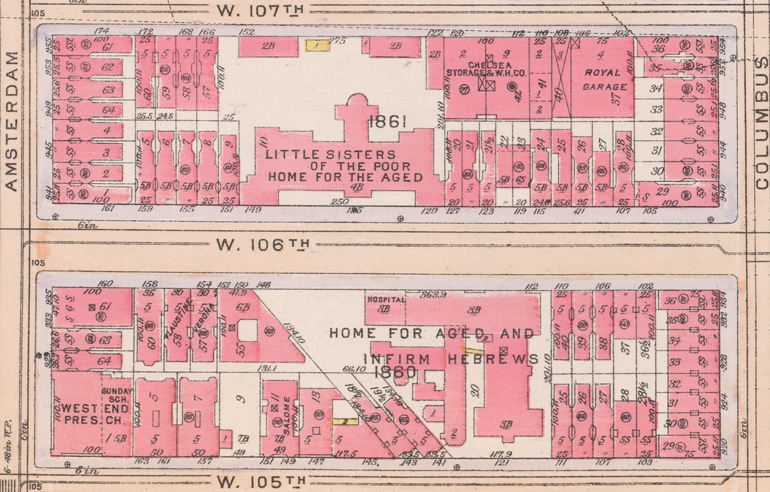
A perennial balance between “home” and “institution” has defined the history of the New Jewish Home. Formerly called the Home for Aged and Infirm Hebrews, its Manhattan campus is an architectural palimpsest. Conjoined yet discrete high-rises of nine and seven stories abut West 106th Street, but behind the institution’s public façade, facing 105th Street, is the first-story of the Home’s 1883 neo-Renaissance brick structure. Though now painted white, its arched entryway and ornament — not to mention its original metal fence — endure.
Originally, the Home for Aged and Infirm Hebrews, and many comparable senior facilities, operated similarly to a palatial boarding house. These private, charitable institutions dotted the American urban landscape in the wake of the Civil War. In a pre-Social Security era, they were established to serve those “worthy” seniors who lacked familial support and hoped to avoid the dreaded almshouse. An applicant was vetted not only in terms of their health condition, but likewise their moral character, and often had to submit references from fellow church and community members. Jews (along with Catholics and African Americans) were often denied access to Protestant homes, finding recourse to simply erect their own eldercare institutions. The New Jewish Home originally served German immigrants, the earliest wave of European Jews to arrive in the United States; by the turn of the century, the facility supported a new migratory rush of Eastern European and Russian migrants fleeing the pogroms.
Though founded as early as 1848 by the B’nai Jeshurun Ladies’ Benevolent Society, the Home for Aged and Infirm Hebrews did not operate as a physical shelter until 1870. The home began on West 17th Street, eventually migrating up to 32nd Street, then 63rd Street, followed by 87th Street, and, finally moving into its first purpose-built structure on West 105th Street in 1881. The home had purposefully relocated from the high-density orbit of its downtown community, chasing what little undeveloped land remained on Manhattan Island. In the absence of modern gerontological or geriatric thought, seniors were said to benefit from the “restful salubriousness” of a suburban setting. This was perhaps an unintentional and early form of social distancing, albeit it at the expense of segregated seniors. Institutional relocation to the urban fringe was common for many old age homes, not just in New York, but in cities such as Philadelphia and Chicago as well.
Residents lived in single or double rooms, partaking in communal meals and recreational activity, all beneath the watchful eye of a “matron” (today, this position is often referred to as an “administrator”). Equipped with a smoking parlor and sitting rooms, the Home was meant to evoke middle-class gentility. There was no allotted medical space; instead, residents would be seen by a volunteer house-call doctor, or otherwise be taken to a nearby hospital. This vision of a mannered and restful refuge for seniors’ final years was hard to maintain, however. Even by 1887, “rapid building operations” adjacent to the Home for Aged and Infirm Hebrews were reported to “nearly [hem] in the premises and [shut] out that open breathing space so much enjoyed by all.” And although miasma theory (the idea that noxious air could cause disease) has since been debunked, the increasing density of life in and around the Home for Aged and Infirm Hebrews meant closer contact to contagion, particularly in an era before vaccines.
Outbreaks within old age homes were common, as were quarantines to protect seniors from outside contagions. One of the first solutions to mitigate the spread of infection from within the Home was to construct an infirmary wing that was adjacent to, yet detached from, the 1883 structure. In 1889, the Home began construction on this V-shaped hospital “pavilion,” an early attempt to segregate the sick away from the more “domestic” milieu of the original building. While the pavilion wings were initially narrow open corridors, equipped with cross-ventilation systems, the hospital would later add “isolating rooms,” which were perhaps intended for more contagious patients. By contrast, in today’s New Jewish Home of Manhattan, all rooms serve residents with a medical, physical, or therapeutic need. Residents are also typically given the privacy of their own bedroom and bathroom, or at minimum a double-room for recuperating.
The New Jewish Home’s architectural past likewise coincided with the Sanitary Movement — a broad public health endeavor that pinpointed urbanization, immigration, and industrialization (and their tenements, factories, and slums) as the baleful causes of smallpox, cholera, and influenza. Outbreaks of these diseases occurred on an almost annual basis within the Home, often because residents wanted to visit with friends and family outside the facility’s four walls. During the 1887 small pox epidemic, the Home’s physician described how “great care was exercised in preventing its introduction among the patients, many of whom thought it was hard they could not receive or call on friends residing in the infected locality.” In 1891, the “grippe,” or influenza, ravaged the Home: “males and females alike succumbed, one after another, the strong as well as the weak yielded,” and “our hospital wards and resources were taxed to their utmost.” The flu would return again two years later. Meanwhile, “a few sporadic cases of cholera” could be traced to Home residents visiting friends in local lodging houses and tenements. “To better protect the old folk” against an 1893 typhus outbreak, “a quarantine was established, and certain restrictions as regarded visiting infected localities imposed, while callers from dubious neighborhoods were excluded.” For nurses, staff, and doctors, the fear of influenza and other contagion was nothing short of routine at senior homes; as the in-house physician at the Home for Aged and Infirm Hebrews declared in 1907, “I concede that I am unable to understand or explain how the specific organism . . . found its way into so large a number of our people.” Nonetheless, “I have long since reached the conclusion that the aged are particularly susceptible to the inroads of this terrible ailment.”
As the history of the New Jewish Home attests, senior care homes have navigated the problem of density for decades. This was certainly a concern during the 1930s, by which time the Upper West Side neighborhood surrounding the Home for Aged and Infirm Hebrews had transformed into a compacted landscape of brownstones, apartments, and tenements. The institution, which served an increasing number of chronically-ill seniors, was at a crossroads over how the facility should evolve in the decades to come, or how to accommodate more people and larger facilities in an increasingly dense urban fabric. It even considered relocating to the suburbs permanently. And yet the Home for Aged and Infirm Hebrews, unlike many of its counterparts, chose to stay on the Upper West Side (it opened satellite campuses in the Bronx and Westchester). The decision to “stay put” in the city was unusual, but as the Home’s president explained in 1930:
“Sight must not be lost of the fact that we wish to provide not alone for the physical needs of the inmates but, in addition, to make our wards as happy as we can, and we would have to consider whether the happiness of our inmates would not be seriously affected if our wards were removed from the city where they can visit relatives and friends and be visited by relatives and friends in return, and were deprived of the city life to which they have always been accustomed, and be compelled to adapt themselves in their old age to rural life to which they are strangers, and which would undoubtedly have a most distressing effect upon them.”
Just as physical proximity could potentially subject vulnerable seniors to disease, social isolation is arguably worse. This remains one of the great lessons that the historic facility has to offer: that the place of eldercare, and its ability to maintain connectivity, matters. Today seniors not only have a visual sense of integration within a bustling city life, but residents are closer to cultural activities and field trips — parades, plays, museums, or even a simple stroll with a health aid over to Central Park — while families and friends, in addition to staff members, are able to access the facility via public transit.
The New Jewish Home’s contemporary slogan — Age like a New Yorker — speaks to the institution’s acknowledgement of the importance of place-affiliation and place-identity to seniors. As Atul Gawande asks in his book Being Mortal: Medicine and What Matters Most in the End, how do we enable wellbeing — “the reasons one wishes to be alive” — without subjecting seniors to a sterilized existence? Keeping older adults in their community “home,” and melded to a social collective, is critical to allowing seniors to age as they have always lived: like New Yorkers.
Yet many senior care homes have always operated within a distinct geographic orbit, often in parallel to the “outside,” intergenerational world. This is why sociologist Erving Goffman labeled them — alongside convents, and orphanages, and jails — “total institutions.” It is an epithet that has stuck, and encapsulates many of the negative reactions we have to visiting nursing homes. But for disabled or chronically-ill seniors, these facilities are sometimes unavoidable. The COVID-19 pandemic has asked an ageist world to empathize with homebound seniors by living a circumscribed life. Let’s hope that sticks: an understanding of just what it means to be homebound, and the limitations it places on a person’s life. One of the future lessons of the coronavirus, paradoxically, is to not keep seniors hermetically sealed from a wider community; that, in addition to protecting the physical health of older adults, we must not forget their emotional need for human connection. This is, to a great degree, a question of architecture, urbanism, and policy.
Perhaps the most obvious and accepted solution is to support seniors in independent living situations for as long as possible — or as long as they wish. Policymakers have recognized this reality for decades, as Social Security and its gradual overhaul throughout subsequent years, including the 1965 Older Americans Act, has allowed many seniors to live self-sufficiently on a monthly benefit package. Providing independence for older adults will also involve the continued allocation of affordable housing for seniors operating on a fixed income, the creation of home units to accommodate elder couples or the widowed, as well as creative strategies to foster multi-generational communities or housing complexes. Nursing homes and assisted living facilities should be envisioned at a much smaller physical scale, to better incorporate them within a community’s built fabric.
In fact, designers and nursing home administrators have suggested just this strategy in reconceiving senior care design for a post-COVID world. Some organizations have advocated for this scheme for decades. The Green House Project, for example, is a decentralized, nonprofit attempt to establish senior environments that meet certain scale, layout, and staff recommendations for “homelike” settings. Even these institutional buildings can be planned with an intergenerational goal in mind. Colleges, including Arizona State University and SUNY Purchase, now play host to senior living facilities on their campuses, while nursing homes and daycares have been conjoined under a single roof, as at Providence Mount St. Vincent in Seattle. The question remains how to hybridize notions of “home” and “institution” within a community, especially when nursing or assisted care is necessary for some older adults. In spite of COVID-19, however, one path is clear: social, spatial, and architectural density, a sense of visual and communicative porosity between seniors and their communities that acknowledges both the medical and the emotional needs of older adults.
Note: Historical quotes are drawn from various annual reports published by the former Home for Aged and Infirm Hebrews.
The views expressed here are those of the authors only and do not reflect the position of The Architectural League of New York.
Comments